Where did it all start?
V1C or virtual first care is emerging as a fresh-faced healthcare solution during an era of social distancing and consumer choice. Over the past year, brick and mortar businesses in many industries, including healthcare, have transitioned to virtual business models to accommodate both staff working from home and patients seeking care from home, to stay safe during the pandemic. Some healthcare providers have moved away from in-person care at physical locations entirely, instead focusing on V1C or virtual first care.
The virtual first approach has the potential to improve healthcare for patients facing barriers to access including those at high risk of complications from COVID-19 or with mobility/transportation limitations. V1C is intended to improve patient access, experience, and outcomes by centering care around the patient rather than around the provider or practice.
In January 2021, the American Telemedicine Association and the Digital Medicine Society (DiMe) came together to form IMPACT, the Virtual-First Medical Practice Collaboration. The goal of the initiative is to lay the groundwork for V1C (virtual first care) and support providers building entirely virtual care platforms.
What is V1C?
On June 15, 2021, IMPACT announced the official definition of V1C: “Medical care for individuals or a community accessed through digital interactions where possible, guided by a clinician, and integrated into a person’s everyday life”. Other characteristics of V1C include:
- The ability to initiate care any time of day from anywhere through digital means
- Care matched to a patient’s clinical needs and communication preferences, combining primarily virtual care with in-person (when necessary)
- Adherence to applicable healthcare laws including upholding care standards, patient security, privacy, and data rights
- Solutions encompassing the entire patient care journey
V1C solutions may include any combination of the following elements, taking a customized, situational approach:
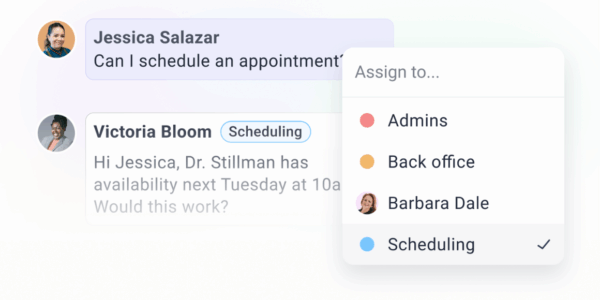
- Synchronous and/or asynchronous patient communication
- A comprehensive approach to health, including specialist consultations
- Prescription of medicine or digital therapeutics
- Patient self-reporting of symptoms and pain
- Caregiver support including digital resources
- Care navigation support
- Mail-in lab tests
- Remote patient monitoring
- At-home sensor technology like blood pressure cuffs and smartwatches
- Digital educational content promoting patient self-management
- Technical support to promote digital literacy and minimize barriers to access
Resources for building a virtual-first care platform
On September 19, 2021, IMPACT announced the creation of the Payer-V1C Contracting Toolkit which serves as a resource for providers offering V1C solutions. The goal of the Toolkit is to help virtual-first care platforms gain contracts with insurers, ultimately expanding patient access to safer, more patient-centric and convenient care.
So far, virtual first care has far outpaced the payer processes necessary to reimburse it. For V1C to become accessible for more patients, beyond just those served under direct-to-patient models, it’s important that third-party payers can contract with these companies as easily as with providers and vendors.
The issue? With traditional contracting, a healthcare solution must classify as either a provider or a vendor. V1C doesn’t fall into either of those categories. Luckily, the Payer-V1C Contracting Toolkit provides a third path payers can take which supports contracts with V1C solutions.
The Toolkit offers an actionable Guide to Payer-V1C Contracting, a Guide to V1C Payment Models, and a Coding Library with V1C-applicable billing codes.
OhMD and virtual first care
OhMD is thrilled to work with incredibly forward-thinking virtual-first care groups like Ayana Therapy, Expressable.io, and Patient 360.