In this episode of “The Patient Conversation”, telehealth consultant Sam Lippolis and OhMD CEO Ethan Bechtel share their expectations for the future of telehealth and suggest best practices for delivering patients the best telehealth experience. They cover the importance of nailing down workflows, training providers on technology, and educating patients to adapt to a hybrid care model.
Transcript:
Ethan Bechtel: [0:00:10] All right. So today we’re talking to Sam Lippolis, who I met through Clubhouse of all places, and got to know her and her experience in telehealth, which isn’t new experience. She’s been doing it for a lot longer than all of us. And so she’s a wealth of knowledge on the telehealth front.
And so I’m really excited to talk today and get more of your thoughts on, you know, what’s been happening in the past year and where we think things are going to go. And so… gosh, where do we start? It’d be great to get from you just a high level, based on what we’ve been through in the past year, what have you seen in the past year that in all of your experience in your time in telehealth, what is exciting you the most about what’s happened in the past year, as it relates to telehealth?
Sam Lippolis: Awesome. Well, Ethan, I’m psyched to be here today. And yeah, we met on Clubhouse, which is just such a funny thing that now we all get to connect in this, I call it like the only social media I’ve actually ever enjoyed. So it’s fun to then make these real human connections, which is what’s different than a lot of other things. Yeah, so most exciting in the last year… I’ve been in the telehealth space for 11 years. So 10 of them was at large health systems as a telemedicine director.
And then the last year really working as a trainer, consultant, advisor for different groups. And this might sound really simple, but what’s most exciting is that now, the majority of clinicians have been exposed to telehealth and more than just exposed, they actually had to do it.
There’s been a big difference. I mean, the decade that I would go into department heads or go into big meetings with different clinicians, I mean, people are always like, “Sam, we’re going to kill someone. We’re not doing that. That’s a terrible idea. This will never work. Patients won’t like it, it won’t work. You know, we’ll hurt people.”
And I think what we’ve seen over this year is that’s not the case. There’s so much we can do remotely. And so for me, that is what’s most, it just might sound dorky, but what’s most exciting is that now all these clinicians have touched it, seen it. And it’s hard to say, “Oh, it doesn’t work,” after a year of actually doing your practice that way.
What’s the future for telemedicine usage by healthcare practices?
Ethan Bechtel: [00:02:43] I can’t imagine how different that is than what you had done over the last, you know, 10 plus years. Right? Like, I know that in my experience, knowing people that have worked in telehealth in large health systems, it was a lot of work to get people to buy into the idea. Like the concept of telemedicine as something that can scale within a health system wasn’t something that was easy to convince people of.
And I feel like there’s some analogous path here to the electronic medical record in the early days when we were implementing it. I did a lot of that and it was the same kind of slog. Like “What? How? I today speak into a Dictaphone and then it just comes back and it’s magic. Why would I want to do all of this other stuff?”
And then there was this tipping point. It feels like the last year has been this tipping point, which to your point, it exposed everyone to this thing. They had to do it in some way, shape or form. And so they were exposed to the value. Is that kind of what you’re seeing in the work that you’re doing today?
Sam Lippolis: I think yes and no. I mean, I think one of the challenges that probably I realize about myself is that I’m always pushing farther. Like I’m like, well, what’s the next, what’s the next? So what I’m looking at right now is seeing that during the pandemic, the data, you know, we had 80% televisits. And now if we look at health systems, and I’m not talking about people who do things in the employer space because we see different data there…
If we look at health systems now, they’re dropping back into this 20% zone. And people are saying, “well, it’s how it has to be.” And I’m instantly, like, “that’s not how it has to be. That is business as usual.” That is before we were all remote. And so we really had to continue to use these tools to connect, and now the practices are open again, or the hospitals are open again.
And because there’s not a good understanding of how to integrate and have a true hybrid kind of model. Then I think we see the 20% just out of people who are like, I don’t want to come in and they’re like, “Okay, we’ll do tele”. So I look at it much more like now let’s look and see what’s the right tool for the right patient with the right kind of thing.
So is that email? Is that texts? Is that phone? Is that video? How do we, again, make this much more the care continuum instead of these sort of transactional interactions?
And if we look at the data of organizations that work directly with employers, so they may have an onsite clinic and then they have tele tools also, they went also 90% tele, but they’ve come back at a 40%. And I think 40% is the right number. And they would include that of everything: email texts, phone calls, video. I think that’s the right number. In the employer space they probably have a little bit easier of a path because of payments, but we still have good payments here and it’s not only about the emergency waivers, which, you know, we could dig into deeper.
So I think, yes, but I think we still have a long way to go because clinicians are… and, I love them… but they are adverse to change. And so you change cause you have to, but if you open the doors back up and we don’t keep the momentum of how this is valuable for patients and for clinicians, then going back to business as usual is really easy. It’s just a habit.
Choosing the right tool for the right patient in the right situation
Ethan Bechtel: [00:06:10] Yeah, so that makes sense. You’re really making me want to skip ahead to like a question that isn’t even here. I’m going to come back to that. That’s related to the employer telehealth that’s happening today and where we expect that’s going to go. So that’s not even on my list of questions, but I’m definitely going there in a minute.
As we think about going into the second half of 2021 and we’re starting to see a majority of American adults have been vaccinated or at least had their first shot. I know you said 40% is the number you expect things to land at. When do we hit the 40% number and is that something you think will continue to creep up as comfort level and maybe competitive forces drive practices and health systems to think more about telehealth as a part of their core model?
Sam Lippolis: Yeah. So that’s a good question. The 20% number is where we’re seeing it land right now and that’s actually also the number that like Advisory Board and Sg2 had been predicting for like five years. Saying like, “hey, 20% of ambulatory could be done tele”. And of course, pre-pandemic, we were probably like two, maybe three, if we’re lucky, five.
So the 20% was already predicted. And what I like about this other organization landing at 40… and I’ve heard some docs who are very open to telehealth saying, “yeah, I could see us landing more 30 to 40”… is I think again, if we look at it of the full scope of the tools: email, text, phone, video, if we just think about everything remote, then really, if people actually looked at their practice, the amount of emails they send and phone calls they make, they probably are already that high. They’re just not quantifying it in that way.
So I think what, what we’ll have to see is, again, is really truly the care continuum? How are we addressing each patient’s needs along the path instead of like, “Oh, you need an appointment? Okay, come in.” Or, “oh, get on video instead”.
Is it a triage? Is it an algorithm? Is it something that helps a patient know the right tool? And is it even as simple as on the website? “Oh, for A, B and C, just shoot us an email. For this, we’ll have a phone call.”
You can’t only have it be on the provider side. You also want to help the patients to understand what kind of tool is the right tool for this particular, whatever. So, I think it still takes a while because it’s still change. And if we think about what hospitals are dealing with right now, they’re still dealing with COVID.
They’re still dealing with COVID units. They’re still dealing with like, “Oh my God. How many visitors are allowed to come in here?” Or even in the clinic space and practices, they’re still thinking, “are these people vaccinated?” So I think in medicine right now… in actual physical clinical spaces, they’re still figuring out, “please don’t have anyone come here with COVID. Please don’t get COVID.”
I think their focus is still there. So these more higher levels where you and I come in and we’re like, hey, it should be the whole care continuum. Won’t this be great? They’re thinking “lady, I need to manage PPE and COVID” so it may take a bit of time for that to settle at that number.
But as long as we keep the concept that this is all possible, I think we can get there. And honestly, I also think patients have to push for these things. Because it’s very easy to go back to status quo if your patients aren’t saying they want it.
Ethan Bechtel: That makes sense. For us, we work with a lot with private practices, practice managers, physician owners. Those types of folks. Which many of them just had to make quick decisions to implement telehealth, whatever that meant for them, wherever they’ve landed, as quickly as possible to solve these immediate problems.
It feels to me like, this is a slow transition back to normalcy, right? This is certainly not an overnight thing as we learned. It’s going to continue to transition slowly back to normalcy. And physicians and practice managers in those, you know, small to mid-sized practices are gaining, it seems like, a lot of experience, bumps and bruises, what works, what doesn’t. So that when things settle back down and they don’t have to consider PPE necessarily to the same extent they have been, or, you know, not bringing someone in with COVID, that they would still know what they need to a certain extent.
Right? Is that how you think about it? And then I guess, to follow up… What are the biggest challenges for those types of groups that they’ve been running into as they’ve tested different platforms or implemented whatever they needed to solve a problem today or tomorrow?
Sam Lippolis: Yeah, I think, as you said, this slow transition, I think you’re right, because everyone’s learning the skills now. And I think what’s interesting as I work with clients, whether it’s, you know, an FQHC or a Medicaid clinic where, you know, everyone always says, “Oh, the Medicaid patients… It’s the digital divide. They can’t handle anything.” And my people are like, “they all got on Doxy the last year, it’s going fine”, or whatever platform they’re on they’re like, “It’s going fine. We have some issues”.
Workflows in telehealth implementation
Sam Lippolis: [00:11:48] But I think what’s been interesting is now they actually look at some of their programs with telemedicine in mind. So for example, one client, I’m helping them do diabetic self-management. The 10 week group class. And they’re like, “yeah, we can do that all telemedicine.” I’m like, “you sure can!”
Now there’s different dynamics in a group telemedicine class, but I think what’s great is that people, yes, are seeing these things are possible and now it helps them look at their other programs and say, “oh, you know, what can I do here?” So absolutely, like I said, it’s possible and now they can work for it.
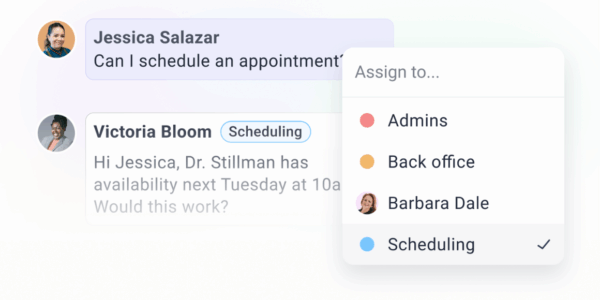
I think some of the challenges that I see and it could be also, cause this is really an area of expertise and something I’ve always been pretty obsessed with is I really see workflows as a big thing. Because if we roll out the tech, but we didn’t actually have a way that we’re sure the patients know how to use it, then what happens is then the doc spends five minutes trying to help the patient figure out how to use it, which is like a terrible use of the doctor’s time.
So these workflow things and how do I make sure, you know, has my patient confirmed the appointment? Like even sometimes appointment reminders can tell them an address to come to.Well, if it’s virtual, you don’t want them showing up, right?
So really the workflows of it. And then also this idea of what can I treat, how? Or if I’m doing a video visit and I need to palpate something, can I do that? Can I tell the patient to do something and that gives me enough information? Even simple things like, I want to see your wound, but then the patient’s kind of holding the phone like this. It’s like, “no, man, turn the camera around, right?”
Like these are very different experiences, but if no one trained you to it, you don’t know. So I think now people are using it and I really see this next year as our time to go back and really dig into the workflows and the clinical training. So that it’s as streamlined as it is in their practice when they’re doing things in person. Yeah.
An approach to creating a hybrid telehealth and in-person model for patients
Ethan Bechtel: [00:14:01] It’s interesting, because I’m assuming that in your time in telehealth you dealt mostly with the implementation of the telehealth practice, right?
Like less hybrid… for some hybrid, from time to time, but probably less hybrid, more focused telehealth. And then we landed in this place where like, it has to be hybrid. Which most vendors didn’t design… no one designed for COVID, first of all. So that’s abundantly clear, but, the hybrid model is hard.
The workflows are really hard and there’s no benchmarks, at least not that I’ve seen lately for this is the specific ratio of telehealth to in-person, for this particular specialty, for this particular geography or demographic age range, right? And so it’s really hard to figure out the balance because everyone’s kind of figuring it out on their own. Right?
It feels like everyone’s just kind of feeling their way through it to see what works. Trial by fire.
Sam Lippolis: Yeah, I think that’s a hundred percent right. Now, I have traditionally implemented hybrid because we were in big health systems or multi-specialty practice and we were oftentimes, because we were using old rules of rural restrictions, we were partnered with rural locations. So it was a way to get rural patients, a lot of times, into specialty care at a distance.
And so one rule of thumb I always give practices when we’re talking video visits and you have a hybrid model is I actually don’t say block out time, unless, you know, you have the volume for it. Otherwise you lose time, right? You’re like, “I could lose time.” So I always ask them this. “Does your practice run on time?” It’s okay if they don’t, because it’s very normal. And if they’re like, “no, not really,” I’m like, “Okay. Well that’s super normal.” So what we suggest is putting your first few appointments of the day as telemedicine, as video visits, and your first few appointments after lunch.
And that allows you to really know you’re on time, right? Right at the beginning of the day and right after lunch. Because the reality is, a patient sitting on a video for 30 seconds or two minutes waiting feels like four hours. So you’ve got to be on time. And so a little fix, like that can make a big difference.
And those same video slots, you can release them 24-48 hours in advance, if they’re not full, to have an in-person. So it could be appointment number one is in person. Appointment number two is video. Appointment number three is video and appointment number four is in person. But that’s one way I always suggest as an easy way to make it a hybrid model right out of the gate is just be open with yourself if you run on time. And if you don’t, it’s totally cool. But just stack those at a time that you’re most likely to be on time.
Ethan Bechtel: Okay. Yeah, that makes sense. That begs the question for me, the idea that it feels like forever if you just like waiting there for someone to join something. Most telehealth platforms, I think, and this isn’t just telehealth, EMRs did the same thing, right? Like let’s design the product or the software around the physical workflow that we are used to today. So the virtual waiting room concept of, you know, let’s make a patient click on this thing, land on this screen, and then they’re just sitting there, like they would be miserably in the waiting room. Let’s recreate that.
We sit there with our team thinking, like, “how do we reinvent that?” Like, that’s an awful experience. No one wants to sit there waiting for someone else. Just like they don’t want to sit there in the waiting room. What are your thoughts on that and how have you seen that done well?
Sam Lippolis: So I haven’t seen it done well yet, so that’s room for you and everyone out there. I mean, actually I’ve thought about that a lot, cause I’m always like, you got to get on here people. But I mean, a lot of people talk about “it’s a great time for patient education”.
I’m sort of like, I don’t know. I don’t love sitting in the clinic lobby watching those, you know, “what I should eat now” either. So like maybe it could be more fun. Maybe it could just be joke of the day. Maybe it could be something fun or like a riddle or like something that will make you a little bit curious.
But honestly I would not be for just more patient education. No one’s going to pay attention anyway. It’s going to be boring. And in fact, apparently there’s this Facebook group or whoever they are… some group of people who make jokes. I’m not going to say what company it is, but a company that gives them various alerts.
And they’ve said like, you know what, I’d rather just have like a joke of the day, or something, than this particular health alert you’re sending me. Because if you send it to me, I know it’s from you. So it will already make me think about that. Like, have it be more fun! So I might actually go more to fun than to just more education and maybe pop in some education. But you know, have some fun.
I even think about ATM’s. So if you’re in New Zealand and you go to an ATM and it doesn’t work, he has this frowny face with his head exploding. And it just says “I’m knackered.” Which is like the best thing. And you’re like, “oh, you poor ATM. Okay. I’ll go somewhere else”. So make it more fun than all this traditional, like, “oh, are you eating this bin of vegetables?” Like, I’m not going to be interested to hear that either.
Ethan Bechtel: At least one of those things you used to see in every pediatric office with the little wooden blocks on the wire. Like maybe a digital version of that I can click around and like drag these things. You know, but at least it feels a little bit more fun than sitting there doing nothing.
That’s really interesting. I have been curious about if anyone has really solved for that. All I can think about, day and night, is how can we build for the patient, first? Right? And you and I have talked a little bit about this, but how do we focus on building for the patient based on where they find value in this healthcare experience and making them sit there doesn’t feel to me like the best patient experience. I think we can do better.
Sam Lippolis: Yeah. Yeah. And I actually even had, I think on Twitter, someone said something along the lines of, “yeah, we’re having this problem because the patients keep hanging up after waiting for 10 minutes.” And I was like,” well, it’s not a problem for the patient. That’s a problem for you.”
You can’t be 10 minutes behind. So this is also a thing that’s very different in medicine, right? We’re used to someone just sitting first in the lobby and then in the clinic room, that’s why those magazines are in there. So we also have to think if I’m doing this, especially a video visit, then that has to be a time that my expectation is I’m on time.
Ethan Bechtel: Yep. Makes sense. So I guess switching gears a little bit, when you think about getting patients comfortable with video or like holding their phone in the wrong direction to show their arm or whatever it happens to be, we focus a lot on texting and the low kind of threshold to understanding how all of the technology works and maybe using that as an on-ramp.
Have you seen practices that start down the telehealth path ease their way in this direction? You know, maybe don’t go straight to video, but they say, “alright, well, let’s start to digitally communicate with our patients more in the portal or using SMS”. And how have you seen success when people all start to walk down that path rather than go straight into video?
Sam Lippolis: Yeah. So that’s a great question. I think what’s interesting is in larger health systems, they tend to be pretty conservative on things. So you basically have a portal and then you go straight to video. Of course now with COVID, things will be different. You will have had emails and things like that, but certainly everything’s through the portal. Texting has always totally freaked out health systems.
I think for private practices, I think here’s where we have all these great opportunities because there are HIPAA compliant tools. And we could just implement that, right? Like it’s actually not that complicated.
So I haven’t actually seen where people are kind of the stepping stone. And probably because when we looked at it through a reimbursement lens three years ago, it was either in-person or video. That’s all you got paid for. Two years ago, although people think it was only ‘cause of the pandemic, it wasn’t, it was two years ago. Two years ago, we started paying for email and telephone calls.
And then with the pandemic, Medicare paid for video from a patient’s home, which made all the difference. So I haven’t seen that progression, but what I can tell you I’ve seen in terms of getting people adopted to things, is, yeah. If you’re starting with text, and let me just put it this way, whether I’m trying to get someone on a portal, or I’m trying to get them on a video, if I have them in person, that’s my entry point.
“Hey Mrs. Jones, did we get you set up on the portal today? That’s so great. Let’s take this five minutes to do it,” because the practices who just hand you a piece of paper and say, “oh my gosh, be sure to get signed up on the portal. Here’s your piece of paper.” Well then Mrs. Jones leaves, she never gets to sign up on the portal. And then you’re frustrated when you try to email her and she’s still not on the portal. And so what I’ve seen over and over again, whether it’s literally “did you download the app so that we can connect through video? Did you download the portal?”
What works best is spending five minutes to have your patient actually do it in the office with you. It sounds goofy. It sounds too good to be true. But it’s real. And so also, if you were totally remote, I would literally have a scheduler. I would script a scheduler or my front office person. Someone who is super nice and talks to patients all the time.
I would give them a script and they would call all my patients, to be like, “oh, Mrs. Jones. We have this amazing new feature. It’s in our portal and you can text us and we could do video visits. Do you have time now that we could just download this to your phone?” Literally, that’s what I would do, because I think this idea that we’re just going to hand humans pieces of paper or mail them things, and then they’re going to want to do it, they’re not going to.
So if we help them get it started and then we’re like, “great! Oh my God, you’re in the portal! I’m going to send you a quick test text. Did you get it? Oh my God. That’s so awesome. Okay, cool. So from now on that’s how we’ll be communicating with you.” Done. And it does feel like more work, but think of when it’s time to get our oil change, we get a text from the oil people.
Dentists. We can look at the dental business to know how we should actually be communicating with patients. It’s all remote. And it has been for a long time. They have HIPAA compliant rules. So I think we have to kind of look other places, but you know, to get people first on the technology: high touch. It’s exactly the same for the providers. They need a lot of high touch to first know how to use it and to feel comfortable and also how to guide their patients how to use it.
Ethan Bechtel: Yeah. So I totally agree with all of that. Obviously looking to other industries that have done it well, I mean, dental is the closest parallel. Obviously the biggest difference is reimbursements and how they get paid, right? And so they’re running slightly different businesses based on, you know, less insurance, more cash, which there’s incentive to create efficiencies, to get patients back for more things. And the dollars are directly attached to the service which is, I think, why so many of them tend to look like good business people because the dots are closer, easier to connect, between the visit, the service and the payment.
But that makes a lot of sense. And I guess my next question around getting both the patient and the physician or clinician to use telehealth: There’s a big element of trust that I think about when you have an in-person care provider and you see them in person, like you get to know them.
Creating patient comfort and building trust with telehealth
Ethan Bechtel: [00:26:00] How does telehealth work to enable or, or kind of make trust potentially more challenging to achieve on both sides? And, and what are the hurdles that need to be overcome to kind of establish that this is a real relationship and that the patient can trust that this is a real visit and the provider is a physician is giving them what they need. And they’re walking out of this visit feeling like they were well taken care of.
And I guess on the other side that the physician trusts that they’re able to diagnose and treat patients as well over telehealth as they are in person. What are the hurdles there?
Sam Lippolis: Yeah. I mean, I think that’s an important one. One, if you had no relationship in person, then part of that is really, if your first one is, you know, let’s say your first one is video, then you really want to make sure you’re spending time to have this eye contact to connect to someone. You don’t want to be like “this feels less personal”, right?
There are some really simple things or everybody’s like, got their cameras, like this. “I’m like, what are you doing? This is not helpful.” Right? Oddly enough, you have to train that. It’s not natural, necessarily that people think about those things.
I think the other way that you can gain trust is if you do have the ability to use all the tools, the texting, the video… things like that, is that the more touch points you have the more of a trusting relationship you’re going to have. Right? So if patients can feel like I ask questions, I get them answered, no matter how those answers come, that’s going to make a big difference and make it feel trustworthy.
I think also for providers to be able to trust that they can treat what they need, I think it is always smart to start with a scope that they’re comfortable with. So whether we pick these 20 things or, you don’t do this, right?
When the pandemic started, one of the peds groups I was working with… it was just determined they didn’t want to do… it was like wellness visits or this certain kind of visit that they really felt was super hands-on. They just decided “we’re not doing that”. And I was like, “okay, cool.” Let’s just not do that.
What happens over time is that the more the providers use these tools, their comfort level goes up. And so I’m actually an advocate of “keep it in the scope you’re comfortable at now. And then start pushing a little bit later”.
“Oh, are you ready for this? Are you ready for this? Like in specialties, some specialties might want to only start with follow-up patients. Okay. Because that’s where they’re going to be comfortable. But as they start to use the tools, they’re like, “Oh, well, you know, if they only have this and that, and I have these tests, I could do that as a new patient.”
“Oh, cool. Okay. Let’s start to do that.” So I think sometimes truly helping them, that’s where you dig in on the clinical language, you talk to them about, “well, what about this disease? What would you need?” And also helping them have conversations, having the clinicians have conversations about “what would you need in person?”
And if they tell you everything they would need, then you figure out, can we actually give that to you remotely? And if we can’t, then you’re like, “man, this is going to be a little harder.” I think if we approach it from that clinical mindset, it helps the clinicians be more relaxed. And while the clinicians are doing it, if they start with a scope they’re comfortable in, the patient’s going to feel more comfortable because the physician will be relaxed.
Right? We always have to figure out this energy, we’re putting out to each other, right? If I’m all nervous and freaked out because I’m like, “Ooh, I dunno if I’m really going to be able to treat this,” my patient’s going to pick that up and they’re going to be like, “Hmm, I don’t trust this. What’s wrong with this visit?” Nothing’s wrong with it. It’s just, I wasn’t a hundred percent sure if this was the best way to treat this.
Ethan Bechtel: Got it. Yeah. That makes a lot of sense. The experience is so nuanced, right? There’s so many things, so many variables. You think it’s just, you jump on a video. And then the first time you do it, you realize, “Eh, there’s a bunch of things I didn’t think about.” The lighting or the camera, or, you know, the audio or whatever it happens to be, and the comfort level.
I think that’s what, I’ve heard this mostly because of the conversations in Clubhouse, but this “webside manner” phrase being the parallel of bedside manner. And obviously what good physicians, or at least the perception of being a good physician, includes is really good bedside manner. That doesn’t necessarily mean you’re more likely to be diagnosed accurately or that your healthcare is going to improve, but it’s a really important piece of the puzzle when you’re trying to establish trust with patients.
So that makes a lot of sense. There’s a lot to think about. Especially since it was all just kind of thrust at most physicians. And I have to say, I guess I’ve got to figure this out.
Sam Lippolis: I think that’s important, when you said they have to figure it out and it’s been thrust at them, is I really think this next year, spending the time to go back and really look at it clinically will help get that number back up to the 40%.
Because my guess is what happened is there were probably a lot of things that providers of all levels, whether it was nurses, social work, advanced practice docs, got on some kind of video or phone (because a lot of stuff is being done on the phone, not that there’s anything wrong with that) but I’m sure there’ve been a lot of instances over the last year where someone got in the middle of a patient appointment and they were like, “Oh my God, I can’t treat this. I don’t feel comfortable doing this.” And what they were thinking in their head was “If I could have just had them in the clinic, this would have been okay”.
Which then further has this perception of “well I better just bring them in.” So if we can actually kind of go back and reset of “No, no. You probably could have done that if you had been trained to X, Y, Z”, and then they’re like, “Oh my God, I could have done that. Wow. I only wish I’d known that”.
Right? So I do feel like it’s important because we don’t want, we don’t want what negative experiences have happened, where they feel like, “Oh my gosh, I didn’t do as much as I could have”, to then have this overriding concept of what digital health can be.
Understand telehealth return on investment through data
Ethan Bechtel: [00:32:27] Yeah, that makes sense. And as you have these conversations with different practices and then you start talking about telehealth. Obviously the necessity of telehealth at this point has pushed everyone in this direction, but how do you talk about, you know, the reimbursement piece, for example?
Right? Like a lot of that is, you know, dollars to time. What’s the comparison in the telehealth world versus the in-person world. And then how do we balance that with the necessity to see some patients in person or not? I’ve seen some stats over time and they’ve kind of been changing pretty quickly as we understand more of the billing implications of using telehealth.
But what are you hearing now around the ROI and whether it does, or does it make sense as a measurement of time spent?
Sam Lippolis: Well, I think an ROI of a video visit is no different than an in-person as long as you have payment parity, right? So if we really think about telehealth as the vision to like leverage and treat more people. Well, for doing straight up video, we’re not doing that because we’re just exchanging a one-to-one.So as long as you’re still getting your professional fee the same, which I believe we should be, it would be years before it should be any different because it takes money to install all this.It takes money to run it and you’re still running a practice, so you still have a physical space that you’re managing.
But where I think we could really understand the ROI, and no one’s doing it yet, I think we’ll start to see things, is really looking at the overall idea of how much time do you spend on the phone? How much time do you spend on emails? What actually of that could be reimbursed?
Because people weren’t trying to charge those things before. If we really started breaking it down and looking at it, I think we could find the right ROI that would also leverage the right kind of clinician, because there’s probably plenty of emails nurses can answer. Plenty of emails, you know, phone calls nurses can do. Then you can have an advanced practice level. Then you can have a physician level. Those things will take time and it also will take the ability for, and it doesn’t matter if you’re a health system or private practice, but we have to have the ability to see the data.
So we have to understand, do you have encounter types that track phone, email? Can we actually see that data to extract it, to understand the minutes and the time you spend on these things? Some organizations like big health systems, if they have an “Epic”, we can potentially find that data.
So I think if practices don’t already account for telephone and emails in some system, they should have encounters for them so that we can actually go back and examine that data and realize, “Hey man, you’re spending X number of hours on this. Half of this could be reimbursed. The other half, okay we just understand that’s the cost of doing business”.
Like if we could see all that, we can help them understand the ROI better. And this year, you know, same, just sort of that idea since everyone’s in more, you know, we’re still sort of in fire mode. We’re not really seeing it yet, but that’s where I would recommend to any practice, having your encounter in your EMR even though it’s a pain. Have telephone and have emails. So you can actually extract the data and understand how much time you spend on those things.
Telehealth reimbursements after COVID and their implications
Ethan Bechtel: [00:35:56] I guess the next logical question is we’re talking fee for service and we’re talking data. And so we now are beginning to kind of accumulate a significant amount of data around what happens when telehealth is the method in which care is provided.
And in theory, in many of those circumstances the dollars spent to the outcome, it should continue to look better over time, right? We should be able to prove that we’re increasing access through telehealth in ways that we’ve never been able to before, which in theory should drive down the cost of care and improve outcomes.
Where does this all go with value-based reimbursement over the next five, ten, however many years it’s going to take to actually get there at scale? Which I think everyone agrees it makes sense, but there’s always a lot of work to do, and we’re not, we’re not the fastest moving industry on the planet.
Sam Lippolis: Yeah. I mean, I think what’s interesting is if we even like, say in the fee-for-service world of payment parity for telehealth, Like right now, CMS, won’t agree to full video visit parity until they see data, right?
But if everyone goes back down to 20% doing it because they don’t want to be, you know, cause they’re like, “Oh, that’s a hassle. I can’t figure out how to do a hybrid model,” then the data is going to reflect, “why do we really need the telemedicine? Because you were at 80% now you dropped 20%. So do we really need it?” Right? So it’s like, come on, everybody keep doing it. So we can then give the data, because CMS won’t make decisions without the data.
Now in the value-based space, I think what’s cool about the value-based space is that you come at it and not necessarily a health system going after value-based. The problem with hospitals and health systems, they don’t have a good sense of what their actual costs are. I’d ask that question as a telemedicine person.
Well, how much did this clinic room cost you so that I can show you how my costs have avoided something? And they’re like, “yeah, we don’t. We don’t know, things like that.” It’s like, “Oh, that seems weird. That’s not how other businesses work, but apparently that’s how this happens.”
Whereas when you’re looking at someone who did something from scratch who then sells into employers, they’re looking at it much more like, “I have a nurse who does this. I have a diabetic educator. I have a pharmacist. They all cost me X.” Right? And then I know I’m going to give all these other pieces of care. So they look at it like they’re coming more from a, “I’ve got this total cost. I know that I can have this many people on a panel and I know then that’ll require me to do this amount of care, and so I know also I can charge X on a PMPM.” Right?
It’s just a totally different way of thinking. So if I were like a private practice and I were trying to figure out what pieces can be value-based, that’s probably where I would be looking at “Do I know, does literature– does someone, something somewhere, show me that if I get my patient into cardiac rehab…
Like I might look at it this way…So cardiac rehab, if you don’t do cardiac rehab, you will likely need, you know, electrophysical cardiology, you’ll need some kind of procedure to do in the EP lab. If I could find data on how many people have cardiac disease end up needing EP, right? But I know that if they do cardiac rehab, I reduced that risk by X. I’d be working in that space, figuring out, “Okay. That would cost a health plan X because they’ll have so many EP surgeries, but cardiac rehab only costs this. And so if I can get people in a cardiac rehab, then I know the data shows me I reduce their chance of needing a procedure by 50%, 60%”.
So I’d probably be looking at it in that way. And then I’d be like, Oh, great. And if it’s value-based, then I don’t care about Medicare’s thing that I won’t do cardiac rehab from home. And then I’ll just do my cardiac rehab from home. And now I have people more attending cardiac rehab because they’re not having to come into a space and things like that.
So I tend to look at it really backwards. I always want to know, well, how much money would it cost to do all of these really complicated procedures or what percentage of people end up in that procedure? What percentage of people end up in kidney failure? So then how do we work backwards from there?
Ethan Bechtel: Got it. Yeah, there’s so much to think about again, like on a specialty or procedure or diagnosis basis, for how we can deliver more value and improve care over telehealth. And there’s so much to learn. It feels like, you know, again, it’s all about data and how can we effectively determine what the impact has been across the board?
So that’s exciting stuff. I know that, we’ve got a few more minutes and I had to go back to an earlier comment about you know, employers offering care to their employees and using different telehealth platforms and companies that focus specifically on that market.
I think I read, I forget where you posted this. It may have been a LinkedIn post, but you had referenced Amazon care. After the news that came out and I think the point was, I didn’t find it as comment, I’m just kind of trying to remember what it was about, but I think it was about that Amazon Care’s movement obviously to their employees first in probably a longer-term move towards direct to consumer telehealth is a good thing for access. It’s a good thing for lowering the amount of friction to receiving care. And I think about this a lot. You know, what of the second and third order effects of the Amazon scale being applied to healthcare.
And so I see all of the positives. I see a lot of potential areas where like “eeeeh, I dunno what this is going to do for these community hospitals and how are they going to make this work?” But I guess the question is, and we’re all just kind of hypothesizing at this point about what this is going to look like.
Commodifying healthcare – a problem for primary care?
Ethan Bechtel: [00:52:52] But the question, I guess, is everyone has spent the last year in brick and mortar practices and hospitals figuring out hybrid telehealth. Amazon is coming in with, we’re going to assume, direct-to-consumer at some point, telehealth.
What does the competitive landscape start to look like for the brick and mortar practices that now all have some level of experience in telehealth versus, you know, Amazon using tech first, direct-to-consumer, and then starting to figure out how to bring people to your home, in theory, I think is what they’re going to do?
Do practices begin to move faster or push harder toward the better patient experiences that they can provide based on what they’ve learned in the past year? And how do you see kind of all of that playing out?
I guess it’s so much to talk about. We could probably talk about this for hours, but high level, you know, what are you thinking about all of that and the impact is going to happen in the next, you know, maybe five years?
Sam Lippolis: Yeah, I think that the Amazon thing. I said, when they announced the primary care thing, for me, it was more like, “ah. I told you so.” Because people like that, Haven fell apart, that thing sucked. I was like, “I don’t know, man, I wouldn’t underestimate what Amazon’s up to.”
Ethan Bechtel: Totally different. Yeah it was hard to see what was going on.
Sam Lippolis: I was like, “they’re still up to something. Don’t call out Amazon.” And with them buying prescription things and you know. So in one sense, where I think we could all end up with some weird problems is by really democratizing primary care, like is happening with all this direct to consumer and the Amazons.
We need primary care. Primary care really manages a lot of complex diseases. And if we keep democratizing it and making it this transactional one-off appointment kind of thing, which is what the direct-to-consumer model is, it’s no bash on them. It’s just what it is. It’s like, you have something low level, I manage you. You have something low level, I manage you?
The problem is primary care doesn’t make much money. They need that bread and butter low-level to handle the co-morbidity, heart failure, diabetes, depression, anxiety. The patient who comes in that takes, you know, an hour and a half that they’re trying to manage. So my concern is this commodifying primary care is a problem for our health system.
And so something’s going to have to, something’s going to have to give with that. Or do we end up with like this other scope of primary care that are really like complex primary care handlers, right? That are handling all the complex people. But the payment model would have to look way different there because of the amount of time and amount of resource they would need.
So that is one concern I have is let’s be careful about how much we nickel and dime primary care because people probably don’t realize how much stuff they take care of that never hits specialty.
I think what’s interesting in these virtual-first and for practices, I do think what we’ll start to see and you know, for people listening and, you know, Ethan, Clubhouse is an amazing place.
You get to learn things you just never had access to before. And really seeing a lot of this employer space, how they’re doing things and these different virtual-first companies. I think what we’ll actually end up… which can be, this is in the specialty space, and I think this could be really useful for specialists…
One problem specialists have right now is like, you’re a specialist here, but you need a big geography to have a big practice, right? To usually have enough, you need a pretty big reach. And there are some places in the country you’re just never going to have enough humans to get everything you need to go.
So I think what we’ll start to see is actual locations that can do physical exams that connect with lots of different specialties and lots of different people.
So instead of your ENT office needing to have five different satellite offices, because that’s how they get enough people that then have enough procedures, you can just have one ENT office, but who connects to these nodes of telehealth like physical exam centers that, that physical exam center could have ENT it, can have oncology, endo, where it’s like a lot of people feeding in.
So almost like… not coworking, cause you’re only handling one person at a time… but where you could have these sort of nodes where the physical exam is done, but your specialists would be coming in from lots of different places. I think that’ll help our specialties see as many people as they need to see and really get the right patients.
Because one problem we have in specialty, if you have access, but you are going in to see a surgeon… let’s say they had a hundred visits, but only 10 of them are really appropriate surgical visits, that other 90 wasn’t the best use of their time.
So if we can also manage that better it actually does give better access. So I love this idea and I’ve been hearing this lately. How do we actually have these sort of nodes of physical exam places? And I’m not talking to a hospital. I’m not talking some freestanding ED or some hospital.
I’m like some tiny little micro thing that literally knows they’re going to have 15-20 different specialists, plus primary care who beams in and then a human is there to help you with the physical exam. Like I think that’s cool. And I think that’s super interesting because what’s really, really important as we talk about all this virtual, whether it’s virtual-first, hybrid, whatever.
Primary care can be leaders in telehealth post-pandemic
Sam Lippolis: [00:48:19] We absolutely have to be conscious that there has to be a way that we then transition to in-person care. We can’t all just be like, “Hey, it’s all going to be remote. It’s going to be so great”. That’s never going to happen. So we have to have very clear pathways.
And I think for those private practices to embrace the innovation is what’s going to let them lead. The data show pre pandemic that 25% of people would leave their primary care doctor for a different one who had virtual. That was pre pandemic. Okay? Those numbers, I bet now are 50%. So every private practice who embraces the innovation, they’re going to be the ones who stay.
And so I want private practices to know that, “Hey man, this is not actually a way to squeeze you out.” Because the hospitals will not embrace innovation as fast as a primary care. Like private practices could do this quick and easy and they could come out as a leader in, you know. I’m a specialist for this or I’m primary care and I do obesity management or diabetes. So like primary care may need to be primary care and a couple of niches that really, they get known for that niche so they can bring in people and specialties could really… yeah.
It’s patient experience, but embracing the future.
Ethan Bechtel: Yeah. Yeah. I think it’s really exciting to think about that. You know, we change out of necessity. That’s human nature, right? Like someone needs to push us to do something. And if nothing else, I think Amazon is going to solve an important problem at scale because no one has the scale of Amazon, but I think outside of what they do directly, the second and third order effects of this are like, they are forcing everyone else to think about how to provide care differently, to lean into the tools that they can use to provide a better patient experience and ultimately treat patients as best they possibly can with the tools I have access to.
So I always kind of go back to this you know, early days direct to consumer apps for essentially urgent care visits. And I remember looking at the data and, you know, I’ve been through like many of us, you know, more than one medical complication and, and being in healthcare I know how important primary care is to quarterbacking a lot of the other things.
And so I just remember seeing data of like, all right, well, a lot of these urgent care visits through, you know, whatever app it was when they were done with that urgent care visit. 60% of them or something crazy then went to an in-person practice because they might’ve learned something on that visit and it might’ve been worth the $50 to a certain extent, but healthcare is more complicated than that.
And the longitudinal relationship that an in-person relationship can provide is important. It plays an important role. And we, certainly as Americans, are not necessarily getting any healthier. Right now there’s a lot to think about. And so I really believe in this real balance of in-person as a really important element of good care with the convenience and benefits of technology to solve for telehealth.
So I think we’re in an exciting place, you know. We certainly have no shortage of things to think about and try to anticipate where the world is going. But yeah, I really appreciate you jumping on here and talking through this stuff. I mean, we’ve done the Clubhouse thing a few times, but this is the first face-to-face- ish hangout that we’ve had.
So thanks so much for jumping on, and I’d love to do this again sometime.
Sam Lippolis: Yeah, I appreciate coming on. It’s a great conversation. And I think what you said is, you know, you and I are in this tele space and we are also believers there is in-person, right? That’s part of healthcare. So we’re not here to say it’s only remote. It is this combination.
I think it’s an exciting time. Like you said, just to see how all this comes together and you know, it’s not only a win for patients, but it’s a win for providers. I think some of these tools can also help improve providers’ lifestyle and things like that, which is super important.
So I’m excited. Thanks for having me on this is super fun.
Ethan Bechtel: Yeah, of course. Let’s do it again. Thanks Sam.
Sam Lippolis: Thank you.