Across the U.S. healthcare system, providers are increasingly shifting away from one-size-fits-all care and moving toward a more thoughtful, personalized approach. Personalized healthcare centers on treating each patient as an individual, using their medical history, genetics, lifestyle, and preferences to guide more accurate and proactive care decisions.
This shift toward personalization reflects a broader move to value-based care—where success is measured not just by volume, but by patient outcomes, satisfaction, and the efficiency of care delivery. Personalized healthcare improves treatment experiences, builds stronger provider-patient relationships, and enables practices to engage patients in their own wellness journeys.
Whether you’re managing chronic conditions, designing care plans, or simply trying to better understand patient needs, personalization is no longer a luxury, it’s a necessity. And with the right tools, like OhMD for seamless patient communication, personalized care becomes more achievable than ever.
What Is Personalized Healthcare?
Patient personalization focuses on the unique needs of each individual patient and allows clinicians to tailor treatments specifically for them. This approach has been shown to improve treatment outcomes for patients with complex conditions such as cancer. So, what’s patient personalization? Simply put, it’s the practice of treating each patient as an individual, taking into account their genetics and other health factors. This approach has been shown to improve health outcomes for patients with complex conditions such as cancer.
Why Personalized Healthcare Matters
This approach has become increasingly important as the healthcare system moves toward value-based care. Personalized treatment can help prevent disease before it starts, identify early warning signs of chronic conditions, reduce avoidable hospitalizations, and improve patient adherence.
It also fosters a deeper level of trust and collaboration. Patients are more likely to engage with a care plan when they feel it reflects their actual needs and values—not just clinical checkboxes. And when communication tools like OhMD are used to facilitate regular, personalized check-ins, it reinforces that connection between patient and provider.
How Does Patient Personalization Work?
Patient personalization is a technique that uses data and algorithms to improve the care patients receive. It has been used in areas such as surgery, chemotherapy, and radiology.
Using patient personalization, healthcare providers can apply a variety of decision-support tools to identify the patient’s needs, preferences, and concerns. These tools are used to try to learn more about the patient and the patient’s health so that they can be addressed in the most effective manner.
Armed with this patient data, the flow of communication with patients becomes less transactional, more consistent, and more trustworthy. Patient personalization is a method for improving the process of patient care by analyzing patient history, records, and behavior to anticipate future needs, and tailoring the patient’s care to meet those needs.
What does this provider/patient care partnership look like in practice? Here’s an example from the primary care field:
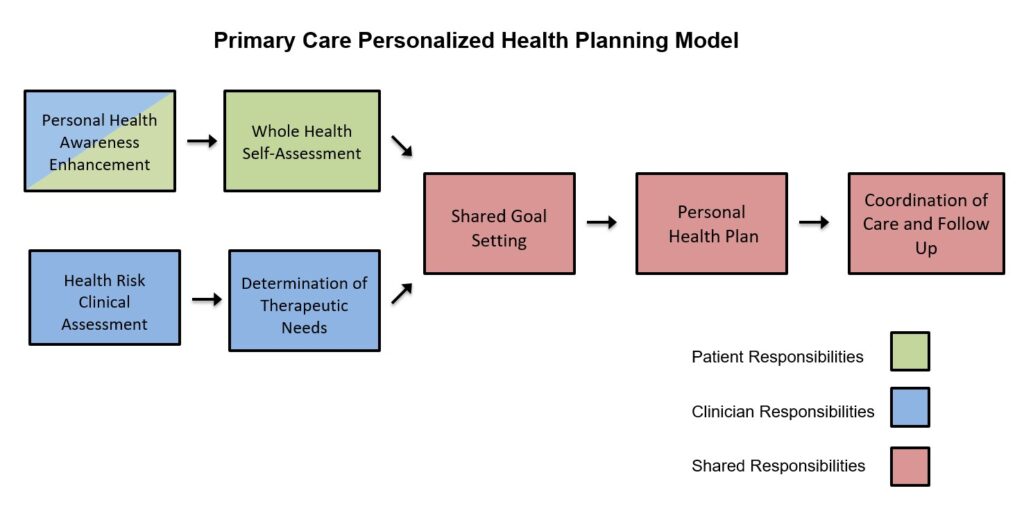
A personalized care plan that is tailored for the patient is increasingly becoming a major focus for healthcare providers and payers as a cost reduction method. Treatment plans customized for the patient that don’t rely on general guidelines cut down on unnecessary treatment, long hospital stays, and a variety of other negative impacts. These cost savings also have impact on the patient as they are better able to manage their healthcare costs. Increases to overall satisfaction can also have impact on reimbursement, so it is in the best interest of providers, payers, and patients alike to consider patient personalization.
Principles of Personalized Care
Several key principles support the shift to personalized healthcare and guide how it’s delivered in clinical practice.
Personalized, Predictive, Preventive, Participatory
This “4P” model involves building personalized treatment plans based on individual data, predicting and preventing disease, and empowering patients to play an active role in their care.
Shared decision-making
A personalized approach includes patients in the decision-making process, allowing them to collaborate with providers and shape their care plans.
Individualized treatment plans
Plans should be tailored to each person’s needs, goals, and life circumstances—not just their symptoms or diagnoses.
Benefits of Personalized Healthcare
Personalized care comes with a wide range of benefits—for both patients and providers. These include earlier diagnoses, lower costs, and stronger relationships.
Improved disease detection
When a patient’s family history, biometrics, and lifestyle are taken into account, providers can detect risk factors earlier and schedule preventive screenings that might otherwise be overlooked.
Lower healthcare costs
Early detection leads to fewer expensive interventions later on. Personalized care also reduces waste by minimizing unnecessary tests, redundant specialist visits, or trial-and-error prescriptions.
Better clinical outcomes and quality of life
When conditions are detected and treated early, patients are more likely to recover fully—or maintain a higher quality of life over time.
Reduced waste and resource strain
Instead of applying generic protocols to every patient, personalized care targets what matters. This can reduce appointment backlogs, unnecessary imaging, and redundant referrals—saving time for both patients and care teams.
Increased patient engagement and trust
When care feels personal, patients are more invested. They’re more likely to ask questions, participate in decisions, and follow through with recommendations.
Risks and Limitations of Personalized Healthcare
While personalized healthcare offers clear benefits, it also comes with challenges that must be carefully managed to ensure safe, effective implementation.
Data accuracy and completeness
Personalized care relies heavily on the availability and accuracy of patient data. If health records are incomplete, outdated, or incorrect, recommendations could miss key risks—or worse, lead to inappropriate treatments. Ensuring clean, comprehensive data is foundational to success.
Risk of incorrect treatment recommendations
When personalization depends on algorithms or predictive tools, there’s a risk of over-relying on technology without clinical judgment. Mistakes in data interpretation or model assumptions could lead to treatments that don’t reflect the patient’s actual condition, potentially causing harm.
Privacy and data security concerns
Personalized care often involves collecting and analyzing sensitive patient data—from genetic information to social and behavioral health factors. This increases the responsibility to protect data from breaches and misuse, especially as more third-party platforms are involved in care delivery.
Equity and access gaps
Not all patients have equal access to the tools or resources that support personalized care, such as internet-connected devices, transportation, or insurance coverage for additional services. Without intentional design, personalization can unintentionally widen disparities between well-resourced patients and those in underserved communities.
Scalability and resource strain
For smaller practices, personalized care can feel resource-intensive—especially when care teams are already stretched thin. Without the right tools or workflows, scaling personalized communication and follow-up may become overwhelming. This is where solutions like OhMD, which automate and streamline patient outreach, can make a significant difference.
Solutions and Tools for Personalized Care
While there are various tools and platforms that healthcare organizations use to address patient personalization, there is no definitive list that clinicians reference as the absolute go to source.
Sources of information on patient personalization tools include healthcare providers’ websites, various associations across different specialties, patient advocacy groups, and consumer review websites like G2.
Places to research patient personalization solutions
Some providers lean heavily on tools like patient surveys, patient diaries, as well as patient engagement solutions. Others rely on homegrown solutions extracting data from their EHR.
Determining the workflows you’d like to address and then choosing tools that are built for a healthcare audience is generally a best practice. As a large part of the personalization of care revolves around building strong relationships, customizing care plans and touch points, a strong patient communication solution is incredibly important. HIPAA compliance and time savings potential for your care team are both considerations one should make as you consider the right solution for you. You also want to think about finding a solution that can provide you a more holistic view of the patient’s needs.
Additionally there are costs associated with switching between various solutions for your team and your patients as data may not easily transfer from one to another. Finally, you want to ensure that your patients will actually engage with your solution so you want to provide them a communication tool little to no barrier to connect with you.
Ready to start texting with your patients?
Let’s chat!
Tools that lead with two-way SMS text messaging, like OhMD are a perfect solution to personalize the care experience for your patients. OhMD allows providers to send patients personalized SMS text messages that contain information about their care, such as dietary recommendations or updates on lab results. In addition to providing valuable information directly to your patients, OhMD also creates a relationship between you and your patients.
With OhMD, you can easily keep in touch with your patients without having to spend time talking on the phone. Providers love OhMD because the HIPAA compliant web-based platform allows them to text patients and have actual conversations with them all from their practice number. The entirety of the patient-provider communication is saved securely in the cloud and can be transferred to the patient’s record in the EHR.
Care team members can also automate common workflows like prescription refills and appointment scheduling outreach, connect over video, call patients, deliver electronic forms for completion and signature right on the patient’s mobile device, and even drive patients to review their care experience on Google and other sites.
What’s Next for Patient Personalization?
Across the United States healthcare industry we are changing the way we treat patients. This is a great thing but it also can present challenges as we continue to improve. By catering to the individual needs of each patient, we can help them feel more comfortable and connected with their healthcare experience. While there are some advantages to patient personalization, it is important to be aware of the potential risks involved. Focus on what you can do well and the tools that will allow you to accelerate toward an improved experience.
Final Thoughts on Personalized Healthcare
Personalized healthcare is transforming the way we deliver care—making it more relevant, responsive, and results-driven. By focusing on the individual, providers can better detect illness, reduce unnecessary costs, and improve overall health outcomes.
Patients benefit from care that truly fits their lives. Providers benefit from stronger relationships, clearer data, and more targeted interventions. And the healthcare system as a whole moves closer to a model that values prevention, satisfaction, and long-term wellness.
With tools like OhMD, personalized care is no longer out of reach. It’s a practical, powerful way to meet patients where they are and help them get where they want to go.
FAQs About Personalized Healthcare
What’s the difference between personalized and individualized care?
They’re often used interchangeably. Both focus on tailoring care to the specific needs, risks, and preferences of each patient—rather than relying solely on standard protocols.
How does personalized care reduce costs?
By detecting disease earlier, reducing unnecessary tests, and avoiding trial-and-error treatments, personalization leads to fewer complications, hospitalizations, and wasted resources.
Do I need special tools to deliver personalized care?
While not mandatory, platforms like OhMD can make it much easier to gather patient data, communicate effectively, and track progress—especially for teams with limited time.
Is personalized care only for complex cases?
No. While it’s especially helpful for chronic conditions, every patient benefits when care is based on their specific history, goals, and concerns.
How can I get started with personalization in my practice?
Start by looking at your intake forms, communication workflows, and follow-up processes. Are they designed to capture and respond to what makes each patient unique? If not, small changes and the right tools can go a long way.




