Key Takeaways: Patient Engagement
- Patient engagement goes beyond showing up—it’s about active participation in health decisions, follow-ups, and ongoing care.
- Strong engagement improves outcomes, reduces hospital visits, and increases satisfaction, but it depends on clear communication, accessibility, and trust.
- Clinics can boost engagement by using plain language, offering two-way messaging, tailoring communication preferences, and tracking key engagement metrics.
Patient engagement is more than just getting patients to show up for appointments, it’s about creating an active partnership between patients and their healthcare providers that spans the continuum of their active health management plan. Patient engagement manifests in small but critical ways, from reading after-visit summaries to texting a provider about side effects and is generally considered a measure of the patient’s active participation in their overall plan of care.
This article breaks down what patient engagement means, why it matters in clinical practice and digital health, and how clinics and health tech teams can increase it. We’ll also examine common roadblocks, practical examples, and essential strategies for enhancing engagement in both in-person and virtual care settings.
What is Patient Engagement?

Patient engagement describes the ways a person gets involved in their own care, whether that’s asking questions during a visit, checking their lab results online, or deciding with their provider what steps to take next. It’s not just about showing up. It’s about active participation.
Still, engagement doesn’t happen in isolation. It’s not something we can expect patients to carry on their own. Providers, clinical staff, and care platforms all shape the experience that either encourages involvement or makes it harder. For example, a provider who uses clear, everyday language instead of complex medical terms is helping build engagement. So is a clinic that follows up after visits with simple instructions (even better if they’re sent by text or available in more than one language). When patients feel supported like this, with personalized care, they’re more likely to stay involved not just at the visit, but in the days and decisions that follow.
Why Is Patient Engagement Matters for Clinics
Engaged patients tend to have better health outcomes. They’re more likely to stick with treatment plans, manage chronic conditions effectively, and catch warning signs earlier. This leads to:
- Fewer emergency room visits and hospital admissions
- Better medication adherence
- Higher patient satisfaction and trust
- Improved preventive care uptake (like screenings or vaccinations)
For healthcare organizations, better engagement indirectly supports operational goals like reducing no-shows, increasing follow-up rates, and strengthening value-based care performance.
Common Barriers That Make Patient Engagement Hard
Despite its importance, many patients face challenges that make engagement difficult. Many patients struggle with health literacy, meaning they may have trouble understanding medical information or following instructions which can lead to perceived non-compliance among a myriad of other possible negative consequences. Others face technology barriers, such as limited internet access or discomfort using patient portals and apps.
Language or cultural differences can also affect how clearly information is communicated and received, especially if interpreters or culturally relevant materials aren’t available. Time constraints are another issue; brief appointments can leave little room for patients to ask questions or voice concerns. In some cases, distrust of the healthcare system, especially among historically marginalized communities, can also make it harder to build meaningful relationships with healthcare providers. Chronic stress or instability, like housing insecurity, caregiving demands, or financial strain, can make health feel like just one more overwhelming task to patients.
Even well-intentioned engagement strategies can fall flat if they don’t account for these realities. For example, sending a long follow-up email might not help someone who struggles with reading comprehension or who only checks their phone in short bursts between shifts.
Real Examples of Patient Engagement in Action

Patient engagement can take many forms across the care journey. Here are some real-world examples:
- A patient uses secure messaging to ask a follow-up question about a new medication when they realize they may be experiencing side effects
- A clinic texts reminders about an upcoming mammogram and receives a confirmation reply
- A care coordinator reviews lab results with a patient and helps them set realistic nutrition goals
- A telehealth provider checks if the patient understood their discharge plan and offers to send a summary via text
- A parent tracks their child’s asthma symptoms using a shared care plan on a mobile app
- A clinic creates a feedback loop by asking patients to rate their visit or flag any unanswered questions
These examples show that engagement isn’t one-size-fits-all. It can be low-tech or high-tech, as long as it helps patients stay connected and actively participating in their care.
Strategies That Strengthen Patient Engagement
Creating stronger patient engagement often starts with simple, actionable changes.
✅ Offer patients clear, plain language communication
Avoid jargon whenever possible. Use everyday terms (like “high blood pressure” instead of “hypertension”) and confirm that patients understand the next steps.
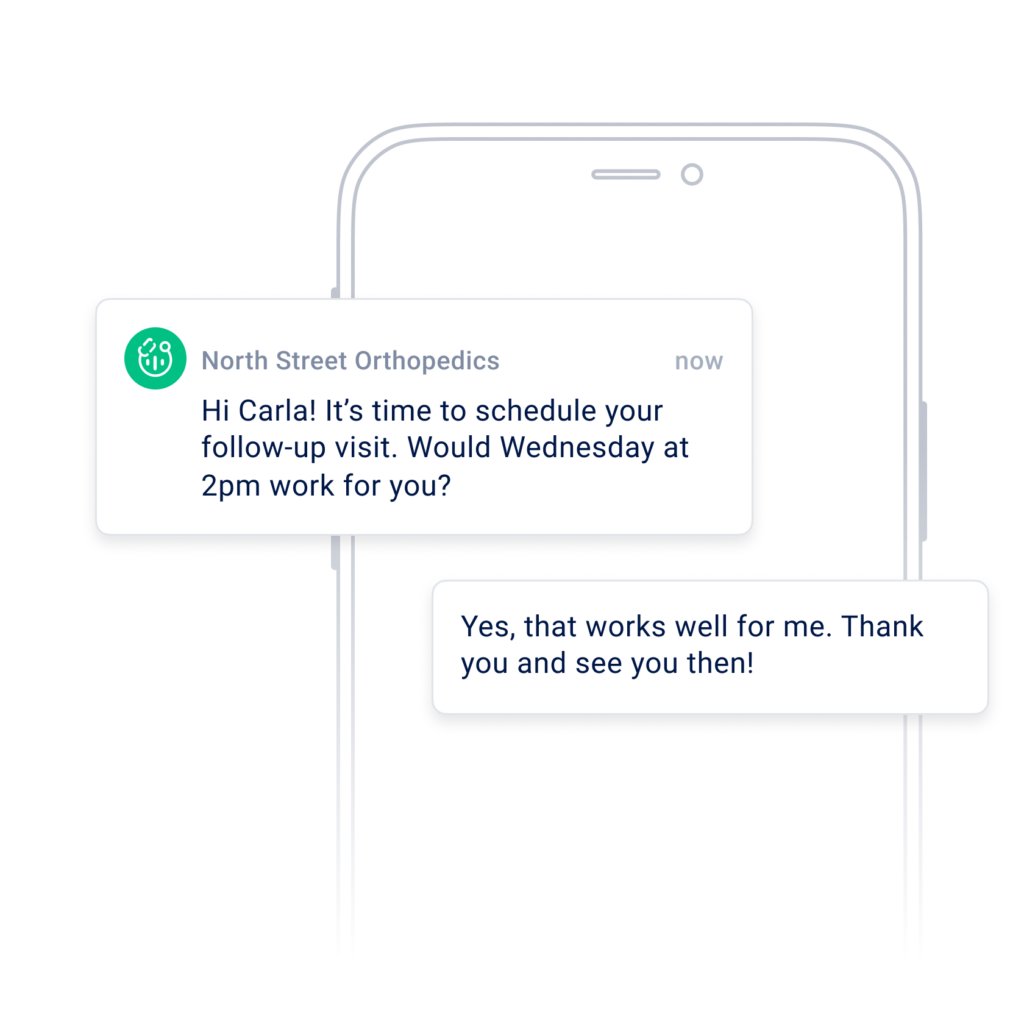
✅ Use two-way messaging platforms
Give patients a way to reply to reminders, ask questions, or clarify details. This builds trust and helps them stay informed without needing to call or schedule a new visit.
✅ Provide access to visit summaries and care plans
Patients forget the majority of what they hear in a visit. Giving them written or digital summaries helps reinforce key instructions (especially when managing chronic conditions).
✅ Tailor outreach to patient preferences
Some people prefer phone calls. Others respond better to text messages. Offering communication options increases the chances of reaching patients in a way that works for them.
✅ Create clear next steps
Instead of saying, “Follow up in 3 months,” help patients schedule the appointment before they leave. For lab tests, include a checklist or instructions about where to go and how to prepare.
✅ Train staff on empathy and engagement in communication
Front desk staff, ancillary staff, and nurses all shape the patient experience. A kind greeting or a moment of listening can go a long way toward making patients feel respected.
✅ Address gaps in digital access
Consider offering printed instructions, low-literacy materials, or personalized tech support and resources for patients who aren’t comfortable using digital tools.
How OhMD Improves Patient Engagement
Visit summaries, broadcast messages, and automated outreach help patients remember next steps and stay on track with screenings, labs, and chronic-care tasks.
Everything is built for HIPAA compliance, with BAAs, audit logs, and secure messaging. Clinics that use OhMD often see fewer no-shows, faster response times, and more confident, engaged patients.
How to Measure Patient Engagement in Your Practice
Tracking patient engagement helps teams understand whether their communication strategies, technology tools, and workflows are actually making a difference. These indicators can highlight both strengths and gaps in how patients experience care.
Patient portal logins or message response rates
One useful place to start is by looking at how often patients log into their health portals or respond to secure messages. This shows how connected they are to the tools available and whether they’re comfortable using them. For example, patients who regularly log in to check results, review visit notes, or send follow-up questions tend to feel more in control of their care. On the other hand, low portal usage (especially in specific age groups or language populations) might point to barriers such as unfamiliar technology, poor user experience, or simply a lack of awareness that the tool exists.
Follow-through on plan of care
Another helpful measure is whether patients complete the next steps discussed in their visits. This might include scheduling a lab test, attending a specialist referral, or starting a prescribed medication. High completion rates often suggest that patients understood the plan and had the tools or support they needed to follow through. When patients don’t take the next step, it may indicate that something got lost in translation. In some cases, they may have misunderstood the instructions, forgotten the details, or run into logistical challenges (like not being able to get time off work or afford the test).
Self-reported engagement surveys
Sometimes the most direct insights come from asking patients themselves. Engagement surveys can ask patients how confident they feel managing their health, whether they felt heard during their visit, or if they know what to do next.
For example, a question might ask, “How confident do you feel managing your condition at home?” or “Did your provider explain things in a way that was easy to understand?” These surveys help surface invisible barriers, such as patients pretending to understand care plans because they felt rushed or didn’t want to ask “silly” questions.
No-show and cancellation rates
Attendance patterns can also tell a story. When patients are engaged, they are more likely to keep appointments and show up prepared. A spike in no-shows or last-minute cancellations might suggest the visit didn’t feel meaningful to the patient or that communication reminders weren’t effective. For instance, if a patient never confirmed a follow-up appointment and then misses it, that could be an issue with reminder timing, delivery method, or clarity (some patients may not realize the importance of follow-up unless it’s explained in concrete terms).
Net Promoter Score (NPS) or feedback comments
Finally, patient comments and survey ratings can highlight trends that aren’t captured in charts or attendance logs. NPS surveys ask whether a patient would recommend the clinic or provider to others, which gives a broad sense of satisfaction. But it’s often the written comments that offer the richest insights. Patients might mention that they didn’t feel rushed, appreciated the follow-up message, or struggled to understand part of their discharge plan. When similar comments come up repeatedly (positive or negative) they can help teams identify which parts of the patient experience are helping engagement and which ones are getting in the way.
Final Thoughts
Patient engagement can be a broad topic, and it’s common to have questions about what it means in practice.
Frequently Asked Questions: Patient Engagement
Does patient engagement improve outcomes for the patient?
Yes. Engaged patients are more likely to follow treatment plans, detect issues early, and feel confident navigating their care. This often leads to better control of chronic conditions and fewer hospitalizations.
What software or tools can help boost patient engagement?
Platforms that offer secure messaging, appointment reminders, care plan sharing, and feedback tools can all support engagement. Text-first tools are especially helpful for reaching patients who don’t regularly check email or log into portals.
Are there any tips and tricks for improving patient engagement in telehealth?
Yes. In telehealth visits, it helps to start by checking if the patient is comfortable with the platform. Use screen sharing or chat to reinforce key points. Always confirm next steps before ending the visit and send a summary if possible (especially if the visit was fast paced).
Patient engagement is a shared process that makes care more effective, personal, and sustainable. Whether through simple check-ins or digital tools, the goal is to keep patients connected to their care and make sure they feel seen, heard, supported, and that they are active participants in their health at every step.
Sources
Office of the National Coordinator for Health Information Technology. “Engage Patients and Families.” Health IT Playbook, HealthIT.gov, U.S. Dept. of Health & Human Services, https://www.healthit.gov/playbook/patient-engagement/.
Agency for Healthcare Research and Quality. Guide to Patient and Family Engagement in Hospital Quality and Safety. AHRQ, U.S. Dept. of Health & Human Services, 2020, https://www.ahrq.gov/downloads/patfamilyengageguide/patfamengagefull.zip.